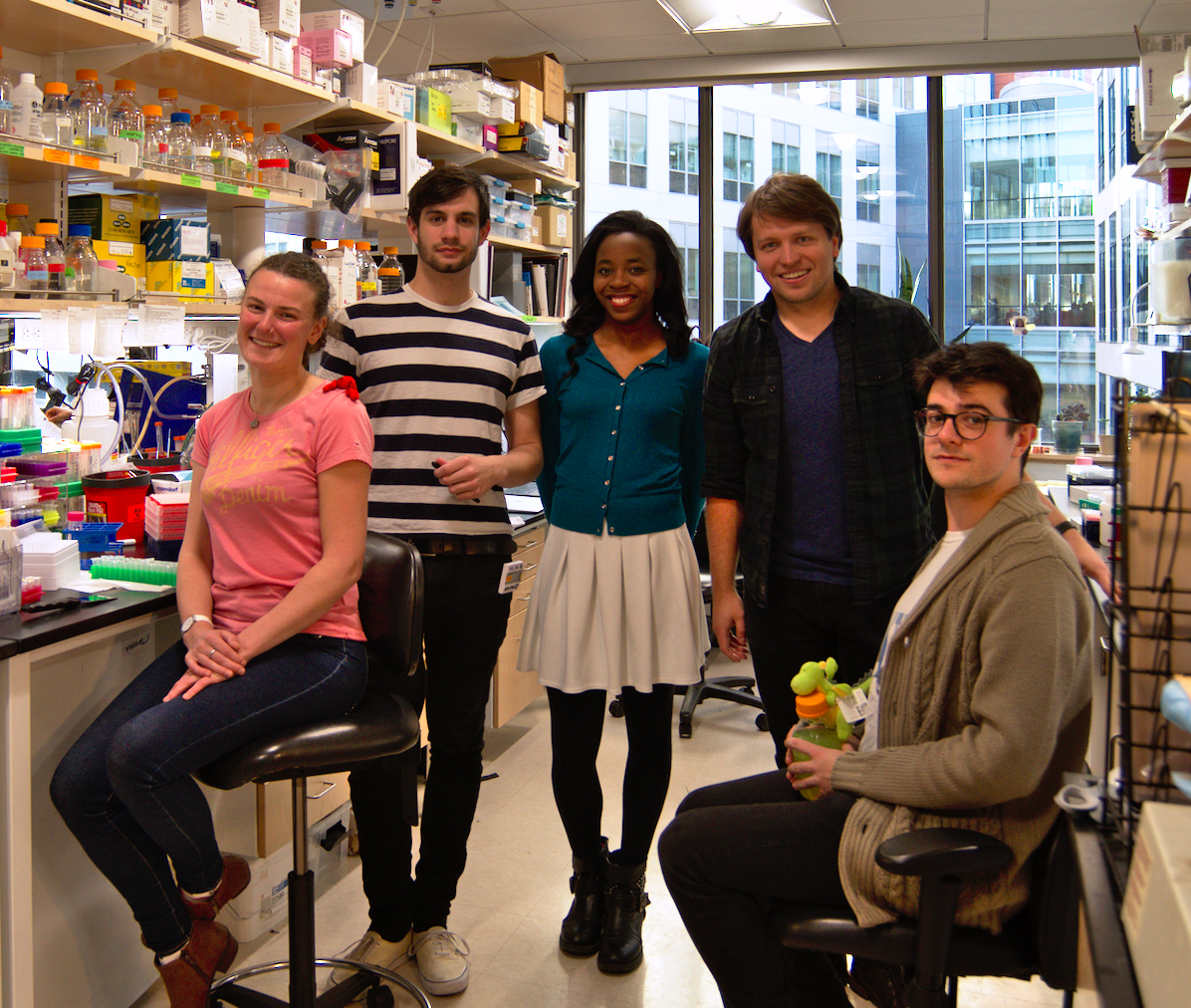
The TSA is proud to be a significant funder to TSC research around the world. We recently partnered with Epilepsy Research Institute UK to unlock completely new TSC research. The lead researcher of the project, Dr Amanda Almacellas Barbanoj, tells us all about her research and the impact that it might have
Dr Almacellas Barbanoj is investigating new treatments for TSC. Here, Amanda explains how therapies that are more specific and with fewer side effects could enable treatment for TSC to start at an earlier age:
Investigating new targets for TSC treatment
“TSC affects around one million people worldwide, and is a rare developmental disorder caused by a ‘mutation’ (error) in specific genes. Our understanding of how this mutation affects development has increased significantly in recent years. People with TSC usually also have epilepsy, and might also have challenges with learning, behaviour, mental health and many other aspects of development. Studying how this mutation affects brain development could help identify new treatments to prevent the symptoms that start during childhood.”
Let’s start at the beginning – how does brain development work?
“The brain has a unique structure. Much like a house has rooms, each one with a specific function, different areas of the brain control different tasks such as decision making, movement or speaking. Many of our genes cooperate to ensure those ‘rooms’ are made correctly, right down to the decorations. Much like how a tile is painted to match the bathroom walls, certain genes control how cells develop into the different parts of a region of the brain. Like how the wiring and plumbing of a house helps to connect all the rooms together in a comfortable and effective home, the same principles apply to a healthy brain.”
What happens in TSC?
“My project looks at how TSC develops following a mutation in the TSC genes (called ‘TSC1’ and ‘TSC2’). These genes are responsible for the direction of the TSC1 and TSC2 proteins, which are important for regulating the speed at which cells multiply and grow, acting like a brake pedal in a car and ensuring cells don’t multiply too quickly.
The group of proteins forming the complex mTORC-1 (mTORC1) are the accelerator pedal increasing the growth speed. Mutations in the TSC1/2 genes disable these brake pedals and keep mTORC1 continuously on, which then instructs cells to multiply and grow out of control. In the case of TSC, the cells dividing into neurons during the formation of the brain instead develop into both benign tumours and immature and disorganised neurons that upset the normal organisation of different brain regions. Ultimately, these defects cause epilepsy alongside problems in cognition (such as learning disabilities), which directly impact the life quality and life expectancy of patients with this condition.”
What is the aim of your project?
“Given the role of mTORC1 in TSC, scientists initially explored the effect of blocking its activity, but were surprised to find this didn’t have the expected strong therapeutic effect. These results pointed towards TSC1/2 as the main drivers of the symptoms of TSC. My hypothesis is that the mutations in TSC1/2 cause a ripple effect in the function of other genes important for brain development.
Therefore, the aim of my project is to explore the other ways in which a mutation in TSC1/2 affects how neurons form and connect with each other. I am cautiously optimistic that this will help scientists gain a better understanding of how seizures and difficulties associated with development, mental health and learning abilities arise in TSC and other neurodevelopmental disorders.
More importantly, this in-depth study of TSC1/2 role in the building of the brain will uncover potential targets of new therapies that could significantly improve the quality of life of the one million people living with TSC worldwide and their carers.”
This blog was originally published on the Epilepsy Research Institute UK website.