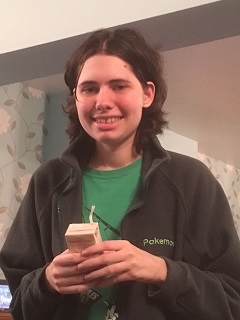
Zoe Clark is 23 and has TSC. She is a bright and verbally adept young woman who loves Pokémon and drawing, and now lives in residential care not far
from her family in Gloucestershire.
Three years ago, however, Zoe was on the brink of death after the rupture of an AML on one of her kidneys.
Zoe’s mum Claire takes up the story. ‘Zoe had only just moved into her own place, supported living,’ says Claire, a nurse. ‘She’d been there a week
when she texted me late one night saying ‘Mummy I’ve been sick.’ I was concerned, but I didn’t really worry unduly as that was all Zoe had said.
I texted back to say ‘I’ll come and get you in the morning.’
When Claire arrived at Zoe’s flat the following morning she was concerned to find her normally chatty daughter looking extremely pale and unwell. ‘We
knew that Zoe had multiple AMLs from a young age,’ says Claire, ‘She had annual scans, with her last one being in 2012 – and we had not been told
that anything had changed – we did not expect a rupture. Having said that, the possibility of an AML rupture is always in the back of your mind.’
‘The biggest challenge with TSC is that so much of it is hidden. Anyone affected by TSC, whether you have it, or you care for someone with it, has
to live with it from year to year – it’s like a time-bomb waiting to go off.
‘And when your child hits their teenage years, with the attendant growth spurts that this brings, this can also cause additional difficulties for people
with TSC.
‘Furthermore, a lot of people have children with TSC who do not have the best verbal skills. So how are you going to know what they are feeling? Looking
back on our experiences with Zoe, I would definitely say to go with your gut feeling – every time.’
Claire has subsequently found out that Zoe’s kidney scan revealed an increase in growth in her AMLs. But she says ‘This information was not communicated
back to me. Looking back, it would have been very helpful to have known that because I would have been much more on the alert for potential ruptures
than I was.’
‘Zoe was white as a sheet and as a nurse I thought she looked in clinical shock. But then, as a parent, you think am I over-reacting to this? I took
her to her GP.’
‘After taking one look at her’ Zoe was rushed by ambulance to Gloucester Royal Hospital. However, petrified of needles and hospitals generally, despite
growing more unwell by the hour, Zoe refused all treatment until a consultant explained that if she did not allow the medics to treat her then
she would die.
‘It was an incredibly worrying, stressful time,’ says Claire, ‘trying to get Zoe to understand the seriousness of the situation was so difficult. And
the worst thing was that Zoe had not complained of either back pain, or blood in her urine, which are the two classic signs we are taught to look
out for in ruptured AMLs.
‘Zoe is very verbally able, but she did not say those things to me, and when I look back I wish that I had trusted my gut instinct more and realised
that something was seriously wrong sooner.’
After successful blood transfusion to replace the 5 litres of blood which had leaked into her peritoneum and embolization under Xray, the bleeding
was finally controlled. Zoe has since made a full recovery.
‘It was a very dark time for us all, but especially for Zoe,’ says Claire, ‘and the emotional consequences of it have taken Zoe a lot longer to get
over than the physical consequences.’
Physically Zoe had to recover from having five litres of blood in her peritoneum. ‘She looked like she was pregnant,’ says Claire. ‘She was so swollen
that she could not lie flat and had to have a pillow and sit up to sleep.
‘The blood which had leaked inside her was effectively squeezing everything, and whenever anything touched her, it was incredibly painful for her.
And for quite a while found that she would have real spikes in her temperature.’
But while time provided a great healer to the physical consequences of her ruptured AML, recovering emotionally took far longer, and, says Claire,
is still an ongoing process.
‘Zoe would have huge tantrums if we asked her to do anything for herself, especially things like cleaning and tidying up. And while things have improved
there are still issues for us to work on, definitely.’
The Clark family attended the TSA annual conference in November 2013 and sought advice from Dr Chris Kingswood, Consultant Nephrologist and the TSA’s
Head of Research Strategy.
‘At that time Zoe had huge AMLs of around 7cms so Dr Kingswood saw us privately in January 2014 and we were, thankfully, able to obtain a private prescription
for sirolimus. And even better, our GP agreed to fund it.’
Since then scans have revealed that the AMLs on Zoe’s kidneys are shrinking, and, ‘apart from a few mouth ulcers’, says Claire, ‘she has suffered no
real side effects from the drug.’ An added benefit has been that Zoe’s facial rash has also substantially reduced, helping her to feel better about
how she looks.
Claire says that if she could go back and change things she would:
‘We are through it now and Zoe is well again,’ says Claire. ‘And I know that while Zoe has been cared for very well by so many nurses and doctors,
I know that everyone affected by TSC would benefit from better regular communication between consultants, GPs and parents.
‘I hope other people will read this and learn from our experience.’




