During global awareness week, and with a focus on ‘World of Thanks’ it is timely for the TSA to show our appreciation of all the work undertaken by TSC researchers globally that over the years have helped enhance our understanding of the condition and develop methods of treatment and management of TSC.
One such team of researchers are based at Cardiff University. The team based within the Institute of Cancer & Genetics have been at the forefront of TSC research over the last three decades. During the 1990s they were responsible for the discovery of TSC1 and TSC2 genes responsible for the disease. Since then they have played a vital role in the development of diagnostics, understanding gene mutations, providing insight to the role of the MTOR pathway in TSC and have lead trials both in pre-clinical and clinical settings.
To celebrate the achievements of our researchers and to build awareness of the work going on in the labs at Cardiff; student Bethan Vaughan went to visit and blog on behalf of the TSA.
Bethan Vaughan
I am currently studying my first year of BSc Genetics in Aberystwyth University. I have always had an interest in science, in particular medical genetics. My interest and curiosity in the subject was further fuelled when my sister, Katie, was diagnosed with TS in June 2009. I attended the 2012 Annual Conference in Birmingham, where I was able to listen to the many talks on the different aspects of TSC which I found fascinating.
I was keen to gain experience in the lab in order to improve my knowledge on the genetic aspects of TSC and expand my laboratory skills. I hope you enjoy my blog!
Lab Experience
Day 1 – Monday
On arrival at the Cancer and Genetics building in Cardiff I met Dr Kayleigh Dodd who showed me around the labs and explained to me what was done in each room. I was given a lab coat and some gloves.
First, I helped Kayleigh with a “Western Blot”. This is a lab technique that allows scientist to separate out and measure the particular proteins they are studying from mixtures of proteins, such as cell extracts. The first step is to load the mixture of proteins into wells at one end of a special slab of gel (a bit like gelatin and pictured below). An electrical current is passed through the gel and the proteins are pulled from the well into the slab. How quickly each protein travels through the gel depends on its size and electrical charge. Big proteins stay close to the well. Smaller ones move more quickly and therefore will be farther away from the well at the end of the process.
The next step is to transfer the proteins from the gel onto a special “sticky” membrane made of a substance called nitrocellulose; it feels and looks a little bit like a thin sheet of plastic. The membrane is placed directly onto the gel and an electrical current is applied running between the two that pulls the proteins out of the gel and onto the membrane.
At this point it was still not possible to see or measure the protein we were looking for. In order to do this we had to soak the membrane in a liquid containing “antibodies” that recognise our protein. Kayleigh explained that the antibodies had come from rabbits that had been immunised with the protein. We then added a second antibody that is able to bind to the first. This second antibody was linked to a chemical signal which meant we could see where on the membrane it had bound.
In our Western Blot, Kayleigh and I were looking to see whether or not a particular protein had been “phosphorylated”. Phosphorylation is one type of modification that takes place within living cells that can be visualised on a Western Blot because it alters how quickly the protein moves through the slab of gel.
Inside cells phosphorylation determines whether certain proteins are active or not and also where they are located within the cell.
Western Blotting is a really important technique because all molecular biologists need to know how to do this. I had never had a chance to do Western Blotting before so it was great (and really very exciting) to get first hand experience!
Next, I went to the tissue culture room and watched Charlie work in a “hood”. Tissue culture is very important because it allows researchers to quickly grow millions of identical cells and study their composition and behaviour, for example how they react to drug treatments or changes in the environment. In tissue culture, scientists grow cells in dishes and flasks inside special incubators that hold a steady temperature (37C) and bathed in air that has an increased level of carbon dioxide. Charlie explained to me the 3 cell models that she is working with; AML cells from humans, embryonic mouse cells that don’t express the protein and rat cells from a rat with TS.
After this, I met Dr Andy Tee who explained to me what research has already shown about the molecular basis of TSC and told me about his current work. Andy also talked me through his discovery that a protein called Rheb is the link between mTOR and the TSC1/ TSC2 complex. I found this very interesting as it increased my knowledge on the genetics of TSC.
I was then introduced to Laura who explained to me how PCR (Polymerase Chain Reaction) works. PCR is a controlled biological reaction in a test tube that allows scientist to take tiny quantities of DNA and make millions of identical copies of that DNA in a matter of minutes – it’s a bit like a molecular photocopier! I then helped Laura and Kayleigh set up a PCR reaction.
Just like Western Blotting, knowing how to set up a PCR is a key skill that all molecular biologists need. So today before lunch I learned 2 really important techniques that will serve me really well in the future!
After lunch, I met Ellie who is researching MPNST (Malignant Peripheral Nerve Sheath Tumor); a disease similar to TSC. I had the chance to ‘passage’ cells with Ellie. Cells will outgrow the space in their container, and use up all the nutrients in the special liquid media in which they are grown over the course of a couple of days. To keep them healthy and alive they need to be diluted out into new flasks with fresh media; a bit like when a gardener splits seedlings in a tray.
At the end of the day, I got a chance to pour the gels for tomorrow’s Western Blots. It’s very similar to making a raspberry jelly at home; the gel starts out liquid, gets poured into a mould and then is left to set. We’ll be using the gels that I poured tomorrow – I can’t wait to get cracking!
Day 2 – Tuesday
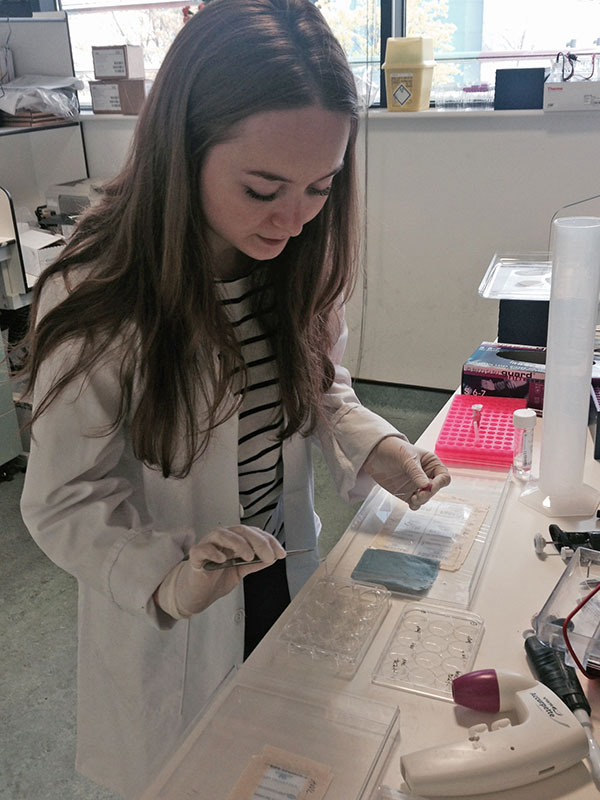
Have you ever wondered how scientists get genes into cells? Well this morning I got to try my hand at this very thing. Sarah explained to me how to do this by incubating the living cells along with the gene we wanted to insert, and then I carried out a few procedures myself (picture).
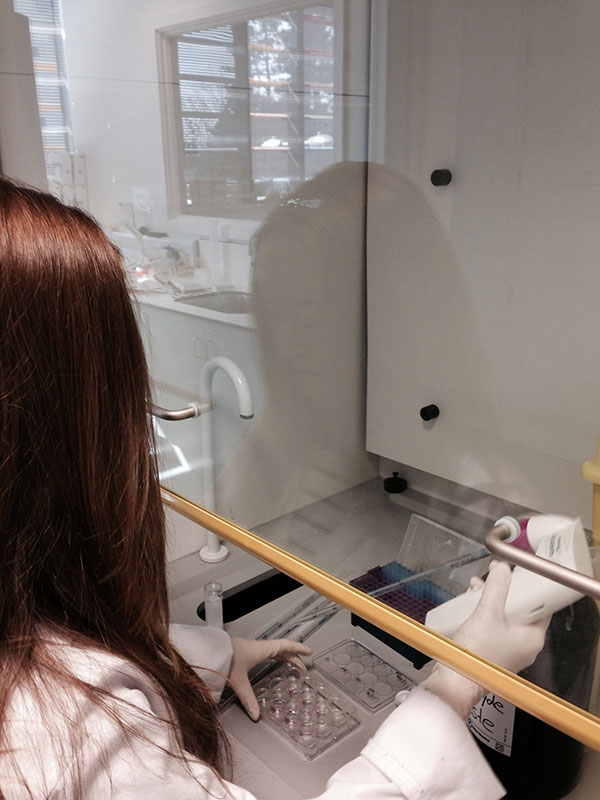
Here (below) I’m working in ‘the hood’ in the tissue culture room. The hood pumps filtered air over the workspace so that no contaminants get blown into the cultures. Everything in here including gloves has to be kept sterile by spraying it with Ethanol and wiping it over before use.
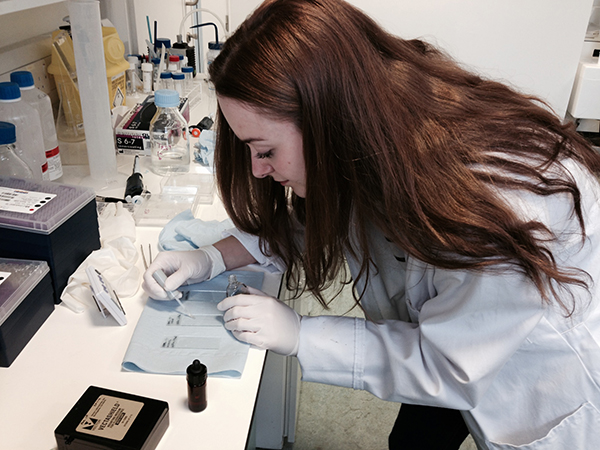
Next, I carried out the second and final stages of Western Blotting with Kayleigh using the techniques that I learned in the lab yesterday. In the picture (below) I am washing the membrane for the Western Blots.
After this, we had a break where I was able to have a quick cup of coffee and socialise with the other researchers. I then attended a seminar given by Charlie on Autophagy, which was very interesting. The word ‘autophagy’ is derived from the Greek “auto” that means “self” and “phage” which means “to eat”. That sounds a bit gruesome but actually it’s the natural process in living organisms that recycles and clears up the components of broken-down cells. I also learned that autophagy is potentially involved in TSC-associated tumour growth and that the group are conducting research into this.
Next, I met Dr Ming Shen, who talked to me about the pre-clinical trials he is working on. Ming showed me a PowerPoint presentation on “Targeted prevention & Therapy of TSC-associated renal lesions in mouse models”. I then had the opportunity to help Ming and Paulina in a new experiment, extracting proteins from tissues or cultured cells by agitating and breaking open them open using very high frequencies of sound. This process is called “sonication” and the machine used to do this is called a “sonicator”. I was able to experience using a sonicator and also the vortex (mixing machine). I also used a machine called a centrifuge which spins the samples very fast – centrifugal force pushes the big chunks of debris that we don’t want to the bottom of the tube allow us to siphon off the cell extra that we want to study.
shows some samples in small tubes called ‘Eppendorfs’. I then helped Paulina analyse the samples in a research instrument call a Spectrometer (below).
Day 3 – Wednesday
Today I went straight to the Medical Genetics building where I met Emer McDermott. Emer is the psychologist screening patients for the TRON clinical study. Emer assesses study volunteers’ behaviour, memory and communication skills. This was very interesting as it allowed me to learn about the psychological aspects of TSC and the range of severity seen between different patients. I already knew that the Tuberous Sclerosis Association is supporting recruitment into this study so it was great to hear more about what it entailed.
After this, I met Dr Anurag Saxena who gave me further information on the TRON study. He also spoke to me about the different phases of the study and explained that TRON was currently in phase II. This means that the researches are focusing on the safety and effectiveness of Everolimous.
Next, I returned to the labs where I learned how to freeze some lung cancer cells in liquid nitrogen with Kayleigh and Daniel (above; Daniel preparing cell samples to be frozen). Liquid nitrogen is amazing (and dangerous) stuff! It is so cold that it could cause frostbite if it came into contact with skin so we wore safety gear whilst working with the liquid nitrogen. Because it is so cold it is able to “snap freeze” cells which prevents them getting damaged. Cells can be stored in liquid nitrogen for a very long time before being taken out, thawed and revived. It’s quite amazing to think about living cells being preserved in this way.
We rounded off the day by treating some AML cells in a dish with rapamycin.
Day 4 – Thursday
The information in DNA is stored as a code made up of four chemical bases (or letters): A, C, G and T. The order, or sequence, of these bases determines the composition of the protein a gene codes for in a similar to the way in which letters of the alphabet appear in a certain order to form words and sentences. Human DNA has around 3 billion bases, and more than 99 percent of those bases are the same in all people. Tiny differences called “mutations” that affect particular proteins can lead to conditions such TSC. So being able to sequence genes is really very important in studying genetic conditions.
Today, I met with Dr Peter Davies who told me all about ‘next generation sequencing’ which is a new technology. Peter explained how next generation sequencing is being used to unravel the fine detail TSC mutations.
The machines analyse the DNA sequence rely on PCR technology (which I learned about earlier this week) and massive computing power. Their use has lead to some really major breakthroughs and I was really excited to see them in action. I was able to observe some really fascinating experiments that show on a computer screen how changes in DNA sequence affect the characteristics of the DNA molecule. You’ll probably have heard DNA referred to as a “double helix”. It is made up of two strands and if you heat up those strands they “melt” apart. On the computer screen Peter showed me how a difference of just one base in a strand of DNA can change its “melting point” (the temperature at which the two strands part) by 3 degrees Celsius. Peter explained to me how this property can be used to study DNA. It was absolutely amazing to be able to see how scientists are able to detect such tiny differences!
After lunch, I went back to the Cancer and Genetics building where I spoke to Sarah about her work on autophagy in Birt-Hogg-Dube syndrome (BHD). Sarah explained a lab technique that she is using called “Site-Directed Mutagenesis”. This technique allows Sara to make specific changes to strands of DNA – it’s possible to change just one base or letter in a strand of DNA. This is really detailed work!
I rounded off my work experience in the lab as I had begun, with Western Blotting. I’m becoming very proficient at Westerns!
I thoroughly enjoyed my week in the labs; there was never a dull moment. I’ve learnt so much and have been able to expand on my laboratory skills and my knowledge of TSC. The whole week was so exciting and everyone I met was so friendly and kind, going out of their way to make me feel comfortable and to make my experience in the labs as informative and interesting as they could. It’s been great to see how TSC research is progressing and really great to alongside TSA-funded researchers at the proper cutting edge! I’ll never forget the experience – a huge thank you from me to the whole Cardiff team.
And a huge thanks from us to Bethan for such an insightful blog and to our colleagues at Cardiff for providing such an action packed week.
To find out more about the research funded by the TSA click HERE
To find about more about taking part in TSC research click HERE