Women’s health
Information on women’s health and living with Tuberous Sclerosis Complex
Most girls and women who live with TSC will experience the same journey in women’s health, such as periods and menopause, as those who do not live with the condition. However, there are some things regarding women’s health that girls and women who live with TSC should be aware of.
The below information covers some of the experiences you may have as a woman, or person with internal reproductive organs, living with TSC. Deborah Holloway (Gynaecology Nurse Consultant at Guy’s and St Thomas) also provided more information and tips on dealing with the menopause at a TSA virtual event:
If you have any specific questions and concerns about women’s health and your specific circumstances, you should speak to a medical professional such as your GP or TSC clinician, as everyone’s experiences will not be the same.
People living with TSC typically start to have periods at the same time as those without TSC, which is usually sometime between 9-16 years old. However, the ways in which TSC might affect someone – such as autism, learning difficulties and/or developmental delay – may lead to periods being more challenging.
Research suggests that one in three women with TSC have an irregular menstrual cycle. Keeping a diary can help to keep track of menstrual cycles. By noting things like how you are feeling, emotions and pain – as well as when you had your last period – it can help you to anticipate when your next period might come and identify patterns. You could do this with a physical notebook, your phone or an app.
Sensory issues related to periods and the menstrual cycle may be an additional challenge for people living with TSC. For example, new odours, witnessing blood or struggles in using products (such as sanitary towels or tampons) could trigger negative thoughts, actions or behaviours.
Periods and other bodily changes during puberty can be especially difficult for people who do not identify as female. Research suggests that people who live with autism (a significant number in the TSC community) are between three – six times more likely to not identify with the sex they were assigned with at birth, compared to people who do not have autism.
You may find it useful to talk about the changes happening in your body (or to talk to your loved one about the changes happening to them). There are lots of resources available to help with this, including books such as ‘The Autism Friendly Guide to Periods’ (written by Robyn Steward, who has lived experience of autism and periods).
If your loved one is non-verbal or partially verbal, you may find visual scales, such as this one, helpful to communicate feelings, such as pain or moods during periods. You might also find social stories helpful for explaining periods and preparing them for them.
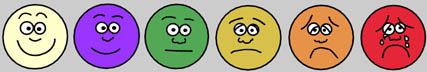
Visual scales can help to communicate feelings or pain
If you live with TSC and epilepsy, your seizure activity might be affected by your menstrual cycle. Some people with epilepsy report a change in seizure frequency at different times of their menstrual cycle, such as at the time of their period, in the middle of the cycle around ovulation, or around a week before menstrual bleeding.
One reason for changes to frequency activity as a result of the menstrual cycle is hormone changes, which is called catamenial epilepsy. You might find it helpful to note stages of your menstrual cycle as part of your seizure diary, as it could aid in identifying if there is a clear link with your menstrual cycle.
If you think that your menstrual cycle does have an impact on your seizure activity, you should discuss this with your epilepsy consultant, who might be able to suggest changes to how you manage your epilepsy to help with this.
You can read more about periods and epilepsy and women’s health and epilepsy from Epilepsy Action.
TSC and LAM
Women who live with TSC and LAM might be advised to not use any hormonal contraceptives, such as the pill. This is because hormone changes in the body can influence how LAM develops. Alternative contraceptive methods include barrier methods (condoms) and non-hormonal intrauterine devices (IUDs). LAM consultants and specialists usually consider that progesterone only contraceptives are safe for women with LAM. They tend to discourage oestrogen containing ‘combined’ contraceptive pills but not progesterone only such as the ‘mini-pill’ or progesterone implants.
TSC and epilepsy
If you live with TSC-related epilepsy and take certain anti-epileptic drugs (AEDs), some methods of contraception may be less effective in preventing pregnancy. Hormonal contraceptive methods such as the pill and implant may be affected by AEDs.
Enzyme-inducing AEDs increase the level of enzymes in the body that in turn break down hormones. This means that hormonal contraceptives break down quicker in someone who is taking AEDs than in someone who is not taking AEDs. If these hormones are not in the body for long enough then they are not as effective in preventing a pregnancy.
If you take an enzyme-inducing AED, you should speak to your TSC/epilepsy consultant or your GP about which method of contraception may be suitable for you.
You can find more information on which type of contraception may work for you based on the epilepsy medication you are taking on the Epilepsy Action website.
Further information
The NHS website has lots of useful information on what contraceptive may suit your needs, but please be aware it is not specific to TSC and you should still speak with your GP or a TSC Consultant.
TSC is a genetic condition, meaning that it can be passed down to children of people who live with the condition. As a result, there are often lots of additional things for individuals, couples and families affected by TSC to consider when thinking about starting or extending a family. You can find out more on our family planning page.
Three in every 10 women living with TSC also have a lung condition called lymphangioleiomyomatosis (LAM). LAM occurs almost exclusively (but not always) in women. Instances of LAM increases with age and whilst only 1 in 3 people may get symptoms, asymptomatic LAM gets more important during pregnancy. It is thought that the hormone oestrogen causes LAM cells to grow (as women typically have more oestrogen in their bodies than men). This means that changes in hormones due to the menstrual cycle, contraception, pregnancy and menopause can all have an impact on LAM. Current research suggests that over half of women with LAM may have a collapsed lung during pregnancy and there may be an increased risk that angiomyolipomas (the most common benign tumour of the kidney) might enlarge rapidly.
mTOR inhibitors are also not suitable (also known as ‘contra-indicated‘) during pregnancy and breast feeding, so please speak to your TSC clinician about this.
Women with LAM who wish to consider becoming pregnant, taking hormonal contraceptives, or fertility treatment should discuss this with their TSC or LAM specialist consultant.
Some women living with TSC may have a higher chance than women without TSC of starting their menopause early. If you have any concerns about TSC and early menopause or menopause symptoms, you should speak to your doctor or TSC clinician.
Due to the link between oestrogen and LAM cell growth, it is not recommended for women with LAM to have hormone replacement therapy (HRT) during the menopause. Your doctor or consultant may recommend other ways to help manage the symptoms of menopause that may be more suitable for you. These could include:
Lifestyle changes:
- Layer clothing
- Avoid synthetic fabrics
- Maintain a healthy body weight and exercise regularly
- Avoid caffeine, alcohol, and smoking
- Identify other hot flush triggers such as stress
Complementary and alternative therapies:
Over the counter supplements are not regulated or controlled in the same way as prescription medication and for that reason they are not recommended for the treatment of menopause symptoms. However, you may want to talk to your doctor or consultant about whether Relizen (also called Serelys or Female) could be a suitable supplement for you to help with menopause symptoms.
Non-hormonal prescription medications such as anti-depressants may also be recommended by your doctor to help relieve some of the menopause symptoms.
You can find more information on LAM, women’s health and menopause in the video resources library from The LAM Foundation.
Download resources
Make a one off or regular donation
£10 Can allow us to send a welcome pack to a family who has just received a life-changing TSC diagnosis, ensuring that they do not go through this time alone.
£25 Can help us develop materials that are included in our support services, flagship events or campaigns.
£50 Can provide laboratory equipment for a day’s research into the causes, symptoms, management or treatment of TSC.
To provide help for today and a cure for tomorrow





